Addiction refers to the continual use of drugs (e.g., alcohol or opiates) or engagement in specific behaviours (e.g., gambling or video gaming) despite the occurrence of psychological or physical harm. According to the United Nations Office on Drugs and Crime, approximately 300 million people worldwide used illicit drugs in 2022, with around 10% showing signs of addiction. This number is a low estimate, however, as it does not include the world’s most abused drug, alcohol. The number goes higher still when behavioural addictions are considered, which are thought to occur at a higher rate than drug addiction.
Historically, addiction has been viewed through the lens of willpower—i.e., addicts lack self-control, unable to control their urges. Not surprisingly, stigmatization and social shunning were the typical outcomes for most addicts. While such views continue to this day, modern research has unequivocally shown addiction to be a disease of the brain (Volkow et al., 2016). It is the result of altered brain chemistry and function, inducing changes in cognition and behaviour.

Read More: The Jellinek Curve: Five Phases of Alcohol Addiction
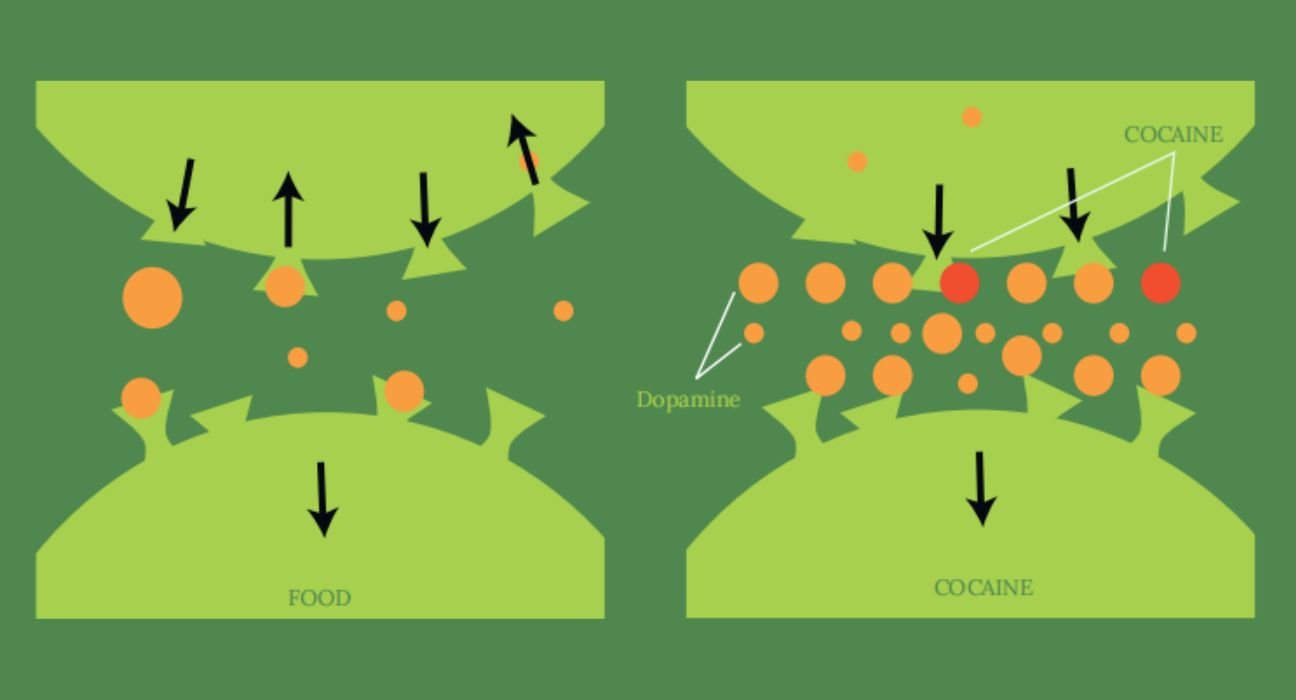
Drugs of abuse increase dopamine
Typically, dopamine increases in response to natural rewards such as food. When cocaine is taken, dopamine increases are exaggerated, and communication is altered.
Two-Stage Model of Addiction
We have developed a new two-stage model of addiction that explores the neurobehavioral adaptations that underlie the addiction cycle — from use to abuse in stage one and abuse to addiction in stage two. The model examines five neuropsychological components of addiction and shifts in the underlying symptomology within each component due to experience-dependent changes in specific regions of the brain. For clarity’s sake, we limit discussion to drug addiction, though the model applies to behavioural addiction as well.
1. Hedonics
The first step in the addiction cycle is simple enjoyment or liking of the consumed drug. A rewarding drug leads to the release of dopamine in the basal ganglia, a collection of neural structures involved in reinforcement and learning. Dopamine release is modulated by opioid and endocannabinoid neurotransmitters, which provide hedonic pleasure to the user each time the drug is consumed (Peciña, 2008).
As drug use progresses, the individual begins to want or crave the drug—providing the necessary motivation to actively seek out more of the drug. This need, or incentive salience (Robinson & Berridge, 2000), is primarily mediated through elevated dopamine release in the mesolimbic ‘reward’ pathway, which includes the basal ganglia, amygdala, and hippocampus. Eventually, wanting can take precedence over the initial liking, such that the individual may not even enjoy the drug they now crave (Berridge et al., 2009). This newfound imperative can have profound consequences as drug seeking and consumption overshadows other aspects of the user’s life (Ikemoto et al., 2015).
2. Learning
The addiction cycle is abetted by two types of associative learning: classical conditioning and instrumental conditioning. The former is engaged when drug effects (i.e., the high) become linked or associated with component stimuli and contexts via the amygdala and hippocampus, respectively (Everitt & Robbins, 2005). For example, alcohol can be associated with a whiskey bottle and one’s favourite bar, whereas heroin may be associated with the needle and building (or specific room) in which the drug is injected. As a result, exposure to cues or environments—even in the absence of the drug—can instigate liking or craving, accelerating the transition from use to abuse.
Over time, there is a shift from goal-directed behavior (i.e., seeking and consuming the drug) toward habitual behaviour. The latter is due to instrumental conditioning, whereby one or more stimuli comes to be associated with a voluntary response and consequence. Hence, the presentation of the stimulus evokes a habitual (automatic) response. Instrumental conditioning depends on experience-dependent changes in the basal ganglia, making the individual less sensitive to negative outcomes (Everitt & Robbins, 2013). In this case, a smoker may observe a pack of cigarettes and, without conscious forethought, retrieve one and light it up. Habits, once formed, are notoriously difficult to break.
3. Tolerance
Tolerance is the diminished response to a drug over the course of repeated or prolonged exposure. Physiological tolerance—wherein drug-dependent dopamine release is diminished and, simultaneously, the mesolimbic circuit becomes desensitized to the dopamine that is available—gradually reduces the effectiveness of the drug (Nestler & Lüscher, 2019). Consequently, more of the drug must be consumed to achieve the same effect or high. Physiological tolerance is thought to counteract the drug’s chemical effects and help maintain bodily equilibrium or homeostasis (Berke & Hyman, 2000).
The cues and contexts associated with a specific drug through classical conditioning can produce an adaptive conditioned compensatory response, maintaining homeostasis, before the drug is even ingested. Behavioural tolerance is an anticipatory or predictive change in body state that counteracts the drug’s forthcoming physiological effects (Birak et al., 2011).
For instance, an experienced user of psychostimulants, such as cocaine or methamphetamine, may experience autonomic depression (e.g., reduced heart rate and blood pressure) when entering the location where the drug is typically consumed. Problematically, the conditioned compensatory response (change in physiological arousal) can be perceived as aversive, propelling the individual to take the drug and neutralize the response (Siegel, 2005)
4. Behavioural Regulation
The prefrontal cortex is critical for a multitude of higher-order cognitive abilities, known as executive functions. This includes the ability to regulate or control one’s behaviour in different situations and settings. As drug use moves toward abuse, the prefrontal cortex becomes dysregulated, impairing its ability to inhibit inappropriate behavioural responses. In as much, the drug user is guided by impulsive decision-making and instant gratification (Poulton & Hester, 2020). A college student that smokes cannabis socially may, for instance, spontaneously decide to smoke a joint by themself before class.
Interestingly, impulsive behavior is not just a consequence of drug abuse; individuals who score high in impulsivity as a personality trait are more vulnerable to drug abuse and addiction (Kreek et al., 2005). As addiction takes hold, impulsive behavior becomes compulsive, defined as performing an action persistently and repetitively with little to no contemplation of the potentially negative consequences. Compulsive behaviour occurs, in part, due to hypofunction of the prefrontal cortex (Lubman et al. 2004), further hindering the brain’s ability to regulate one’s behaviour. Thus, an alcoholic may compulsively continue to drink in spite of significant disruptions to his or her career, relationships, and other facets of life.
5. Reinforcement
Underlying the changes above is a transition in the drug’s reinforcing properties. In stage one, the drug is consumed due to positive reinforcement—liking encourages the user to approach and consume the drug. It is mediated by the euphoria induced by activation of the mesolimbic ‘reward’ circuitry delineated above (Feltenstein et al., 2020). Over time, the user’s behaviour becomes impulsive and the desire to acquire and consume more of the drug grows as physiological tolerance develops. The presence of drug-related paraphernalia and environments further increases longing for the drug and pushes the individual down the addiction cycle.
In stage two, the individual’s drug-taking behaviour is decoupled from positive reinforcement—the drug is now habitually and compulsively taken to counteract the noxious effects of discontinuing its use. Negative reinforcement refers to continued drug use to avoid withdrawal symptoms, due to decreased mesolimbic circuit function and elevated activation of the neural circuitry that controls stress and anxiety (Koob, 2013). Avoidance behaviour is exacerbated by behavioural tolerance, which produces physiological effects akin to withdrawal. With its myriad of symptoms, from stress and fatigue to extreme changes in concentration, appetite, and sleep, withdrawal is the defining characteristic of drug addiction.
Drug Abuse Statistics
According to the Comprehensive National Survey on the Extent and Pattern of Substance Use in India conducted in 2018, the data reveals significant information regarding drug abuse in the country. The survey indicates that alcohol is widely consumed, with an estimated 3,000,000 users aged between 10 and 17, and a staggering 150,116,000 users aged 18 to 75. Cannabis and opioids also show substantial numbers, with 2,000,000 and 4,000,000 users respectively in the younger age group, and 29,018,000 and 18,644,000 users in the older age group. Sedatives, inhalants, and other substances follow a similar pattern. These statistics underscore the need for comprehensive strategies to address substance abuse and its impact on public health and well-being in India.
Conclusion
Considering the plethora of changes inside the brain and their attendant changes to a person’s mental processes and behaviour, it is no surprise so many individuals struggle with addiction. It is not a simple matter of willpower. The two-stage model aims to facilitate the diagnosis of addiction by providing accurate descriptors linking altered brain function to overt behavioural responding. By emphasizing the role of the brain, rather than personality or will, the model is conceived to promote the de-stigmatization of drug addiction in India and abroad.













Leave feedback about this